In 2022, 13.9% of all deaths in the U.S. were caused by heart failure. And contrary to popular belief, it doesn’t only affect older people: Nearly 6.7 million adults ages 20 and up currently have the condition, per the CDC. The good news? Thanks to recent research out of the University of Arizona College of Medicine in Tuscon, there is more hope that heart failure may one day have a cure.
The idea is based on a new study showing that the heart muscle can heal itself — in some cases. Currently, the only treatment options for patients with advanced heart failure are complete transplants or left ventricular assist devices, also called “artificial hearts,” which are surgically implanted mechanical units that help the organ pump blood. Through the research, scientists found that patients with artificial hearts regenerated muscle cells more than six times faster than those with healthy hearts.

“This is the strongest evidence we have, so far, that human heart muscle cells can actually regenerate, which really is exciting, because it solidifies the notion that there is an intrinsic capacity of the human heart to regenerate,” Hesham Sadek, the College of Medicine’s cardiology division chief, said in a statement.
The study identified cardiomyocyte (aka heart muscle cell) renewal in 52 patients with advanced heart failure. The regeneration was “minimal” for those with end-stage heart failure, at between 18 and 50 times lower than the rate for those with healthy hearts, but “significant” for the patients who had received left ventricle assist device therapy.
Why was the difference so stark? For healthy hearts, there’s little hope of regrowth without support from an artificial device. “Skeletal muscle has a significant ability to regenerate after injury. If you’re playing soccer and you tear a muscle, you need to rest it, and it heals,” Sadek explained. “When a heart muscle is injured, it doesn’t grow back. We have nothing to reverse heart muscle loss.”
However, Sadek theorized that the mechanical pump allows the real muscle to “rest” and regenerate, which he likened to a person relaxing and recovering after an injury. Without artificial support, the heart mostly stops growing after we’re born, per a study he published in 2011, since it needs to devote all its energy to its primary function: pumping blood to the body.
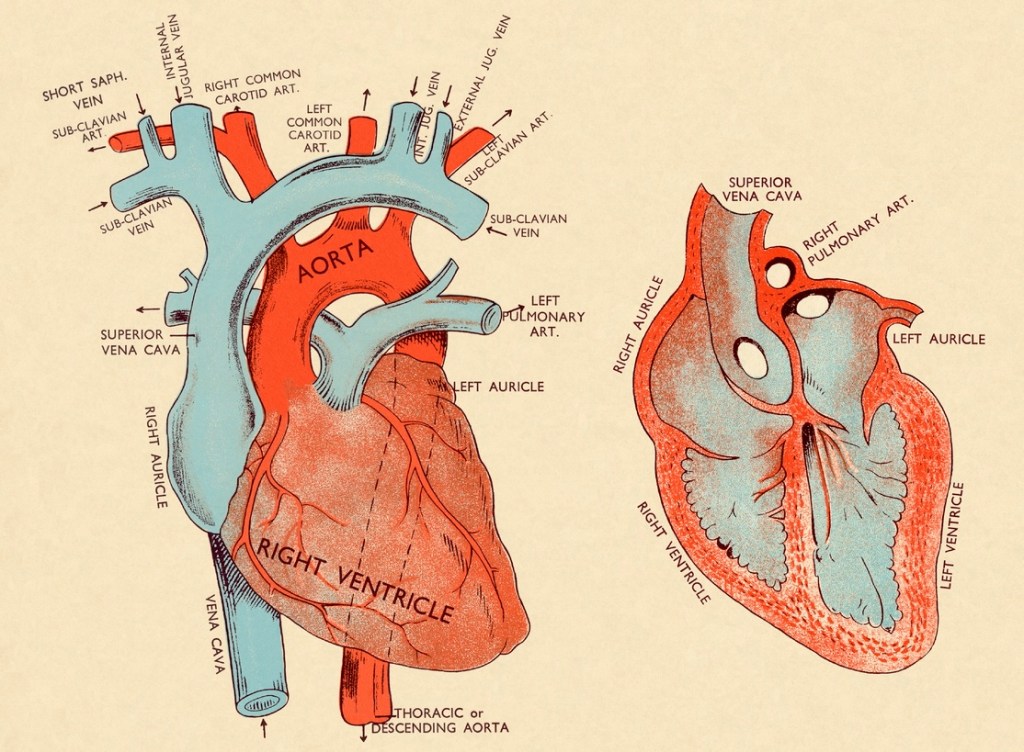
And yet, another Sadek study from 2014 opened the door to the possibility that muscle cells may renew if patients have artificial hearts. In these cases, the devices pump blood directly into the aorta, passing over the heart and giving the real muscle a break of sorts.
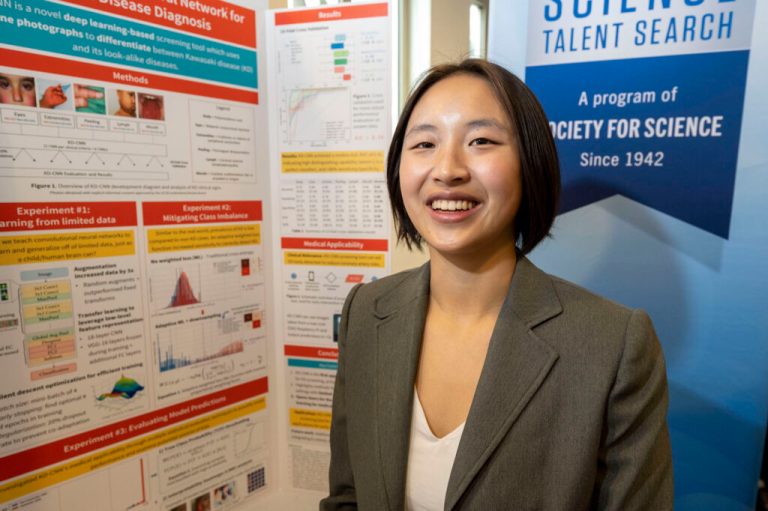
While the previous studies have alluded to these possibilities, the recent research provides “irrefutable evidence of heart muscle regeneration” that “has never been shown before in humans,” Sadek added in the release.
Now, the cardiologist seeks to learn why only around 25% of patients with left ventricular assist devices demonstrate cardiac muscle regeneration.
“It’s not clear why some patients respond and some don’t, but it’s very clear that the ones who respond have the ability to regenerate heart muscle,” said Sadek. “The exciting part now is to determine how we can make everyone a responder, because if you can, you can essentially cure heart failure. The beauty of this is that a mechanical heart is not a therapy we hope to deliver to our patients in the future — these devices are tried and true, and we’ve been using them for years.”
RELATED: Got 10 Minutes? Short Bursts of Activity Linked to Lower Heart Disease Risk